Exploring Cancer Immunotherapy: A Guide to Treatment Approaches
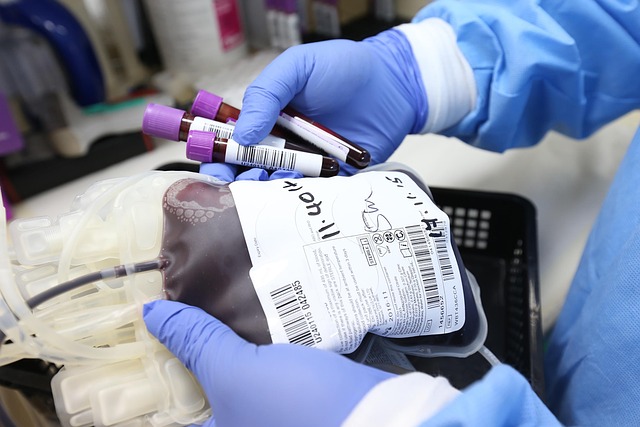
Cancer immunotherapy represents an evolving area of oncology that involves using the body's immune system to target and fight cancer cells. For individuals considering or undergoing this type of treatment, understanding its general principles is often a first step. Some patients report experiencing side effects during immunotherapy, which can include discomfort or specific symptoms. Discussions about immunotherapy frequently involve questions about its potential impact on survival duration, with inquiries varying across different cancer stages. Information is often sought by patients at specific stages, such as stage 1, stage 2, stage 3, and stage 4. Particular attention is given to understanding potential outcomes for stage 4 cancer patients. Immunotherapy is applied across various cancer types, including lung cancer, bladder cancer, prostate cancer, breast cancer, leukemia, melanoma, and colorectal cancer, each with its own clinical considerations and research developments.

Cancer immunotherapy has changed how many cancers are treated by engaging the immune system to detect and control tumor cells. While it is not suitable for every diagnosis, it can be combined with chemotherapy, targeted therapy, or radiation and may help some people live longer with a manageable side‑effect profile. Individual responses vary widely and are guided by tumor type, biomarkers, and overall health. This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is immunotherapy treatment?
Immunotherapy treatment aims to restore or enhance immune recognition of cancer. Tumors often evade detection by exploiting natural immune checkpoints—molecular brakes that prevent overreaction. Drugs called checkpoint inhibitors release these brakes by targeting PD‑1, PD‑L1, or CTLA‑4 on immune or tumor cells. Other strategies include cellular therapies that deliver cancer‑fighting immune cells, therapeutic vaccines that train the immune system to identify tumor markers, and oncolytic viruses that selectively infect tumor tissue. The best approach depends on tumor biology and a person’s medical history.
Immunotherapy cancer treatment options
Immunotherapy cancer treatment spans several categories. Checkpoint inhibitors (for example, PD‑1 or PD‑L1 antibodies) are widely used across melanoma, lung, kidney, head and neck cancers, and more. Cellular therapies such as CAR T‑cell are established for certain blood cancers and are being studied in solid tumors. Additional approaches include TIL therapy, cytokines, vaccines, and oncolytic viruses. Testing can help guide choices: PD‑L1 expression, mismatch repair status or MSI‑H, tumor mutational burden, and driver mutations (such as EGFR or ALK) influence suitability. Clinical trials may offer access to emerging combinations and novel agents.
Immunotherapy for stage 4 lung cancer
Immunotherapy for stage 4 lung cancer is most often used in non‑small cell lung cancer (NSCLC) and, in some settings, small cell lung cancer (SCLC). In NSCLC, high PD‑L1 expression may support checkpoint inhibitor monotherapy, while lower PD‑L1 levels often lead to combinations with chemotherapy. When targetable mutations like EGFR or ALK are present, targeted therapy is typically prioritized, with immunotherapy considered later depending on response and safety. In extensive‑stage SCLC, adding a PD‑L1 inhibitor to first‑line chemotherapy is common. Outcomes vary; careful monitoring for benefits and side effects is essential.
Finding therapy centers nearby
Locating therapy centers nearby starts with verifying that a program treats your specific cancer and offers immunotherapy expertise. NCI‑Designated Cancer Centers and major academic hospitals typically provide multidisciplinary teams, access to clinical trials, and specialized supportive care. Community oncology programs can deliver many checkpoint inhibitors locally, while coordinating with academic centers for complex cellular therapies. Consider factors like coordination between medical oncology, pulmonology or surgery, insurance acceptance, travel logistics, and availability of local services such as symptom management and patient navigation.
Examples of U.S. cancer programs that offer immunotherapy and multidisciplinary care include the following.
| Provider Name | Services Offered | Key Features/Benefits |
|---|---|---|
| MD Anderson Cancer Center | Checkpoint inhibitors, cellular therapies, clinical trials | NCI‑Designated; large thoracic and immunotherapy programs |
| Memorial Sloan Kettering Cancer Center | Checkpoint inhibitors, CAR T‑cell, vaccines, clinical trials | Specialized immunotherapy centers; extensive research portfolio |
| Mayo Clinic Cancer Center | Checkpoint inhibitors, clinical trials, integrated supportive care | Multi‑site access; coordinated tumor boards |
| Dana‑Farber Cancer Institute | Checkpoint inhibitors, cellular therapies, clinical trials | Research‑driven protocols; collaborative care with Brigham and Women’s |
| City of Hope National Medical Center | CAR T‑cell, checkpoint inhibitors, clinical trials | Cellular therapy expertise; accredited transplant and cell therapy programs |
| Cleveland Clinic Taussig Cancer Institute | Checkpoint inhibitors, clinical trials | Strong thoracic oncology; multidisciplinary clinics |
Cancer and immunotherapy: benefits and risks
Cancer and immunotherapy intersect in complex ways. Benefits can include durable responses in a subset of patients and improved quality of life when disease control is achieved. Risks arise from immune‑related adverse events, which occur when activated immunity inflames healthy organs. Common effects include fatigue, rash, diarrhea, and thyroid changes. Less common but serious events involve lungs (pneumonitis), liver (hepatitis), colon (colitis), kidneys, nerves, or heart. Early reporting of symptoms allows prompt treatment, often with corticosteroids or hormone replacement, to prevent complications.
In summary, cancer immunotherapy is a broad set of approaches that help the immune system better recognize and combat tumors. Decisions depend on tumor type, biomarkers, prior therapies, and access to experienced teams and clinical trials. Understanding options, potential benefits, and safety considerations—along with evaluating qualified centers in your area—can help align treatment plans with personal goals and medical needs.